Background:Polycythemia vera (PV) is a myeloproliferative neoplasm associated with an increased risk of thromboembolic events (TEs). PV patients are characterized based on their risk for TEs as low-risk (age <60 without prior history of TE) or high-risk (age ≥60 and/or prior history of TE). Observational studies have shown higher rates of TEs in PV patients compared to matched controls (14.3 vs 4.9/1000 patient years, or PY), with rates as high as 40% in patients with PV (Goyal et al., Blood. 2014;124:4840; Griesshammer et al., Ann Hematol. 2019;98:1071-82; Pemmaraju et al., Leuk Res. 2022;115:106809). We assessed the rate of arterial and venous TEs in a large cohort of low- and high-risk PV patients.
Methods:We conducted a real-world, retrospective cohort study using Optum's de-identified Market Clarity Data, which includes electronic health records (EHR) on 105 million US patients between 2007-2019. Eligible patients were ≥18 years [yrs] old and required ≥2 PV diagnosis codes with ≥60 days between the first and last diagnosis code in the data period. Patients were indexed at the first diagnosis code of PV preceded by ≥1 year of EHR data (“index”) and required ≥1 year of post-index data or death prior to data period end (12/31/2019). Patients with a pre-index diagnosis of secondary polycythemia, leukemia, myelodysplastic syndrome, myelofibrosis, or stem cell transplant were excluded. Patients were stratified into three groups based on risk status at index: low-risk (age <60 without prior history of TE), age-based high-risk (age >60 without prior history of TE) and event-based high-risk (prior history of TE). As outcomes, TEs were identified at the first occurrence of a diagnosis code for a TE in EHR during the post-index period. Descriptive statistics were used to characterize the proportion of patients with TEs and event rates per 1000 PY. Kaplan-Meier analysis was used to evaluate the probability of TE-free survival among patients in the three risk groups at various time points. Patients were censored at death or last engagement date.
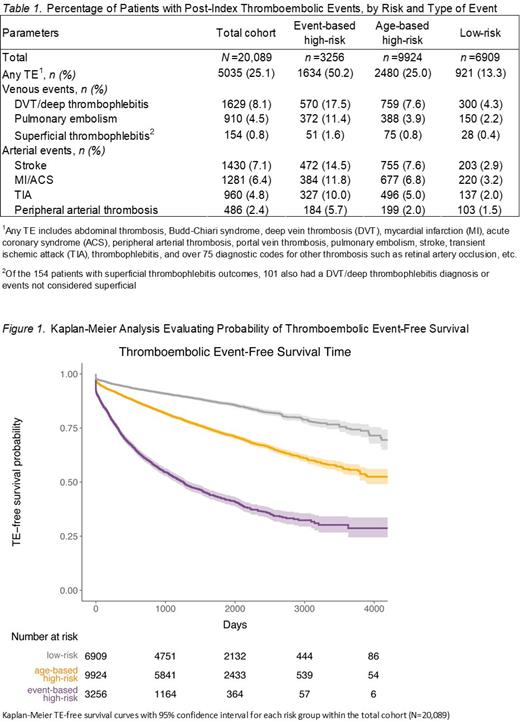
Results:The total study cohort included 20,089 PV patients (mean age, 63.0 yrs; 57.8% male; 88.6% Caucasian). Approximately one-third (34.4%; 6909 patients) were low-risk, 49.4% (9924 patients) were age-based high-risk, and 16.2% (3256 patients) were event-based high-risk. Among 17,402 patients with pre-index medication data, 16.0% (n=2777) received hydroxyurea (HU) pre-index. HU usage was highest in age-based high-risk patients (21.8%) followed by event-based high-risk (20.0%) and low-risk patients (5.8%). Median follow-up period was 4.3 yrs (IQR, 2.4-5.9). Incidence of TEs was assessed within patient groups (Table 1). Overall, 25.1% (5035/20,089) of patients with PV experienced at least one TE during the post-index period. Incidence of TEs was highest among event-based high-risk patients (50.2%; 1634/3256), followed by age-based high-risk (25.0%; 2480/9924) and low-risk patients (13.3%; 921/6909). The rate of post-index TEs was more than triple for event-based high-risk patients vs. age-based high-risk patients (206 vs. 68/1000 PY) and nearly 7 times higher vs. low-risk patients (206 vs. 31/1000 PY). The rate of TEs was more than double for age-based high-risk patients vs. low-risk patients (68 vs. 31/1000 PY). Incidence of arterial and venous TEs was assessed across the total cohort (Table 1). The most common arterial events were stroke (7.1%) and MI/ACS (6.4%). The most common venous events were DVT/deep thrombophlebitis (8.1%) and pulmonary embolism (4.5%). Kaplan-Meier analysis indicated that at ≈2.5 yrs (1000 days) post-index, TE-free survival was ≈90% for low-risk, ≈80% for age-based high-risk, and ≈55% for event-based high-risk patients (Figure 1). At ≈5.5 yrs (2000 days) post-index, TE-free survival had fallen to ≈85% for low-risk, ≈70% for age-based high-risk, and ≈40% for event-based high-risk patients. The downward trend continued until the end of the data period.
Conclusion: Findings from this real-world analysis indicate that PV patients experience high rates of arterial and venous TEs. Event-based high-risk patients have a substantially lower probability of TE-free survival compared with age-based high-risk and low-risk patients. While patients with a prior history of TE have the highest thromboembolic risk, all patients with PV are at high risk of TE, indicating an unmet need for reduction of thromboembolic risks.
Disclosures
Kuykendall:CTI: Consultancy; GSK: Consultancy; Sierra Oncology: Research Funding; BMS: Consultancy, Research Funding; Imago: Consultancy; Prelude: Research Funding; AbbVie: Consultancy; Protagonist Therapeutics, Inc.: Consultancy, Research Funding; Morphosys: Consultancy, Research Funding; Incyte: Consultancy; Blueprint: Consultancy, Research Funding, Speakers Bureau; Novartis: Consultancy. Yacoub:Acceleron Pharma, Inc.: Consultancy; Apellis: Consultancy; Gilead: Consultancy; Novartis: Consultancy; Pfizer: Consultancy; Pharmaessentia: Consultancy; CTI Pharma: Consultancy; Protagonist Therapeutics, Inc.: Consultancy; Incyte Corporation: Consultancy; Servier: Consultancy; Notable Labs: Consultancy; AbbVie Inc.: Consultancy; AbbVie, Acceleron, Apellis, CTI Pharma, Gilead, Incyte, Notable Labs, Novartis, Pfizer, PharmaEssentia, Servier.: Consultancy. Reaven:Protagonist Therapeutics, Inc.: Consultancy. Funk:Protagonist Therapeutics, Inc.: Consultancy. Oyuela:Protagonist Therapeutics, Inc.: Current Employment, Current equity holder in publicly-traded company. Valone:Protagonist Therapeutics, Inc.: Consultancy. Dinh:Protagonist Therapeutics, Inc.: Current Employment, Current equity holder in publicly-traded company. Bellamy:Protagonist Therapeutics, Inc.: Current Employment, Current equity holder in publicly-traded company. Modi:Protagonist Therapeutics, Inc.: Current Employment, Current equity holder in publicly-traded company. Molina:Protagonist Therapeutics, Inc.: Current Employment, Current equity holder in publicly-traded company. Gupta:Protagonist Therapeutics, Inc.: Current Employment, Current equity holder in publicly-traded company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal